Viewpoint by Bilal S., Experienced Consultant at Amaris Consulting
In the realm of medical innovation, gene therapy stands as a beacon of hope, a frontier where science and technology converge to redefine the possibilities of treatment. At its core, gene therapy involves the strategic transfer of genetic material into a patient’s cells or tissues, aiming to rectify the underlying causes of diseases at their roots. Imagine it as a cellular reprogramming, like a software update for our DNA.
Initially tailored to address specific genetic typos causing monogenic (single-gene) disorders, gene therapy took on the role of a genetic mechanic. The original objective was simple: replace faulty genetic components with healthy counterparts, fine-tuning our cellular machinery in the process.
As scientific understanding progressed, so did the ambition of gene therapy. It transcended the realm of single-gene issues to confront more complex challenges, notably the formidable adversary of cancer. Yet, the approach underwent a transformation. Instead of merely correcting genetic errors, scientists embarked on a new strategy, introducing genes with a distinct mission: the targeted elimination of cancer cells.
However, amid the promise and potential breakthroughs, gene therapy encounters an array of challenges. From the intricacies of gene delivery to concerns about safety, cost implications, and ethical considerations, the journey towards unleashing the full potential of gene therapy is not without its hurdles.
In this exploration of gene therapy, we navigate the intricate landscape of challenges that researchers and practitioners must overcome to usher in a new era of medical possibilities.
Two paths, one destiny
In the complex dance of gene therapy, the paramount challenge lies in delivering genes effectively, making sure the genes stay active in the specific cells we want them to be in. This challenge is met by two fundamental strategies: ex vivo and in vivo delivery.
Ex Vivo
In the ex vivo approach, a meticulous genetic tailoring process unfolds. Patients’ cells of interest are collected, genetically modified, and then reintroduced into the patient’s body. Here, special viruses called retroviruses carry a healthy copy of the gene into the cells’ genetic code. This ensures that every new cell made from these modified ones also has the corrected gene. However, the first attempts had a problem – not enough cells were fixed. Recognizing the need for a more comprehensive approach, researchers discovered that they needed to destroy some of the patient’s bone marrow cells before putting in the modified cells. Unfortunately, this process, myeloablative stem cell transplant, can increase the risk of secondary tumor development.
In Vivo
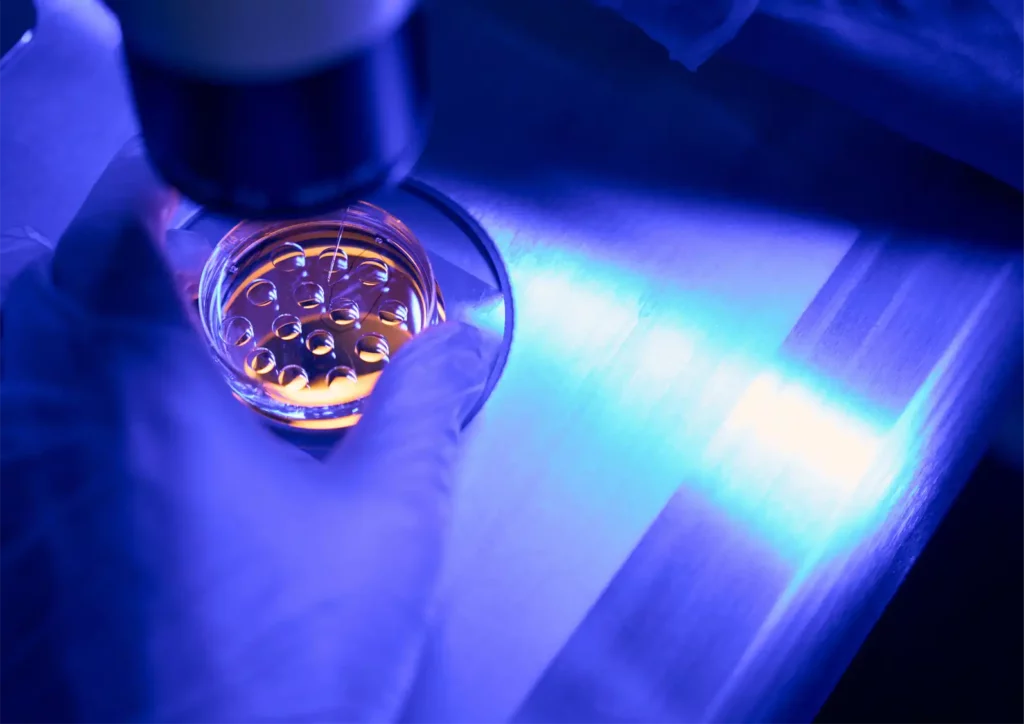
The in vivo approach takes a more direct route, delivering genes either locally at the tumor or through the bloodstream. The challenge here is protecting the genes as they travel through the body. Scientists use carriers like lipids, polymers, or viruses such as AAV (adeno-associated viruses). AAV has emerged as their preferred choice as they infect humans but don’t cause disease. Importantly, the gene delivered by AAV doesn’t stick around in the cells that divide, making it safer
Outweighing potential risks
Gene therapy, like any medical treatment, confronts safety challenges that must be carefully considered to ensure its potential benefits outweigh potential risks before gaining approval. One big safety concern is insertional mutagenesis. This happens when the added gene goes into the host’s genetic code randomly, possibly causing gene problems and diseases like cancer. AAV is used to lower this risk, but research suggests that gene integration could still happen, depending on the dose and which cells are targeted.
Another challenge arises from people already having been exposed to AAV in their lives, developing neutralizing antibodies against them. This exposure can reduce the effectiveness of gene therapy. To address this, scientists exclude patients with preexisting antibodies, use immunosuppressive drugs, or modify AAV vectors to decrease the immune response. This strategic approach aims to enhance treatment efficacy by overcoming the hurdles posed by the body’s immune system.
Balancing innovation and accessibility
Gene therapy comes with a hefty price tag, reaching up to $2.1 million per patient for treating spinal muscular atrophy, a rare genetic disorder causing progressive muscle wasting. The high cost is because gene therapy often requires only one treatment to bring long-term benefits, especially for diseases that were initially considered incurable. This leads to a significant socioeconomic impact, raising concerns about whether gene therapy will be accessible only to those who can afford it.
Acknowledging these concerns, recent proposals suggest outcome-based rebate arrangements for some gene therapies. These arrangements would offer reimbursement if predefined therapeutic outcomes are not achieved, potentially making gene therapy more financially feasible for a broader population.
Ethical questions arise
While gene therapy holds the promise of curing genetic diseases, it grapples with ethical dilemmas, especially regarding the potential modification of germline cells, which can be passed from parents to children.
A key ethical concern revolves around the idea of modifying the germline through gene therapy, which could alter the genes passed on to future generations. Current regulations in Europe and the United States strictly limit gene therapy to somatic cells, avoiding any germline modifications.
In 2015, Chinese researchers made headlines by using genome editing on human embryos to confer resistance to HIV infection. This marked a significant departure from established norms, prompting questions about the ethical implications. The use of non-viable embryos and the unsatisfactory results underscored the need to improve techniques. This raised a host of ethical questions: Should researchers have first tested the technique on animal embryos? Is introducing genetic modifications, even in non-viable embryos, ethically sound? Where do we draw the line between what is considered moral and what is not?
These questions touch on the core of ethical considerations in gene therapy, questioning the boundaries of what is morally acceptable.
With great power comes great responsibility
As we stand at the forefront of a genetic revolution, gene therapies offer unprecedented hope for treating diseases once considered beyond the reach of medical intervention. This transformative power, however, is accompanied by profound responsibilities and challenges that extend well beyond the laboratory and clinic.
Beyond the scientific frontiers, the compass of gene therapy directs us into uncharted ethical waters. The power to mold our genetic makeup calls for a nuanced understanding of the responsibilities it entails. As we explore the potential to reshape fundamental aspects of our existence, let us do so with a commitment to ethical stewardship, ensuring that our pursuit of health and perfection aligns with the principles that underpin our shared humanity.
At Amaris Consulting, we stand at the forefront of innovation, facilitating the responsible integration of groundbreaking technologies to redefine the possibilities of healthcare and life sci